This Universal Health Coverage (UHC) Day, the theme is “Keeping the Promise.” There is no shortage of high-level political promises on achieving universal health coverage (UHC), ending tuberculosis (TB) and leaving no one behind, as well as recognition of the co-dependency of the agendas to end TB and achieve UHC. For example, the UN High-Level Meeting on UHC recognised the need to “strengthen efforts to address communicable diseases including HIV/AIDS, TB, malaria and hepatitis as part of UHC and to ensure that the fragile gains are sustained and expanded by advancing comprehensive approaches and integrated service delivery and ensuring that no one is left behind.”
Moreover, the World Health Organization (WHO) lays this out clearly in the 2019 Global TB Report: “the End TB Strategy milestones for 2020 and 2025 can only be achieved if TB diagnosis, treatment and prevention services are provided within the context of progress towards UHC.” In addition, the required rates of decline in incidence and mortality rates of TB have only been achieved in the context of UHC, combined with social and economic development that reduces known risk factors for TB infection and disease.
But, as the UN Committee for Development Policy has acknowledged, leaving no one behind is “seldom disputed in principle, but the complexity of its practical implementation is often insufficiently acknowledged.” The response to TB, where 30% of new cases go undiagnosed, unreported or untreated each year (referred to as “missing” people), is a good place to start on practical implementation to reach those who are most often left behind by health systems, including with social protection interventions.
Efforts to end TB and achieve UHC go hand-in-hand. Given that the people most vulnerable to TB are often those “left behind” by health services more generally, for example due to social marginalisation or economic status, building health infrastructure aimed at reaching all people with TB provides an important pathway towards achieving UHC. Further, the global move towards achieving UHC, for example through making quality and accessible services affordable for everyone, is an important opportunity to reach all people with TB.

For this reason, social protection and UHC are key components in the new Global Plan to End TB, launched this week in Jakarta. It is significant that the meeting is in Jakarta, given that this year’s Global TB Report found Indonesia to have made significant gains on finding the “missing” people in 2018. This contributed significantly to the decrease in “missed” people globally. This is thanks to scaled up investments and improved strategies that put people are the centre and actively reach out to vulnerable communities.
The need to include social protection support in the TB response is highlighted in the End TB Strategy’s Pillar Two (ensure that health and social sector policies work jointly to address the social determinants of TB). Social protection interventions for people with TB include:
- Financial support: Cash-transfers, stipends or reimbursements help people to pay for the extra costs associated with TB diagnosis, treatment and care. Such as transportation costs for reaching the health services. This is essential to prevent people being pushed into poverty as a result of having TB.
- Nutritional support: 2.3 million cases of TB in 2018 were attributable to undernutrition – more cases than any other risk factor. Among people with TB with a BMI (body mass index) of under 18.5, between 2012 and 2016, the mortality rate was over 50%. People with TB need to have eaten before taking their medication to help keep it down, and nutritional supplements for people with TB can help aid recovery and a return to active life.
- Psychosocial support: Prevalence of depression is estimated to be as high as 50% among people with TB. People with TB who are depressed are three times more likely to stop treatment due to side effects. Mental health services must be integrated into TB care, such as counselling.
- Health education: This is important to help all people with TB to take their medication in the prescribed doses and to understand the importance of completing the course. It also helps with ensuring that people who were in contact with the person with TB are referred for testing or preventive therapy. This can be delivered by community health workers, who are often trusted members of a community and are able to visit people where they live.

Figure 2 highlights the complex interactions between TB and most of the other SDGs. For example:
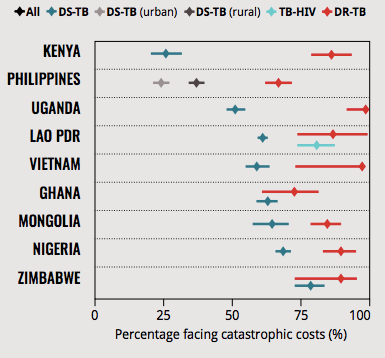
- Goal 1: End poverty and implement social protection systems for all. Ending extreme poverty and expanding social protection coverage would result in an 84.3% reduction in TB incidence by 2035. Countries with higher levels of social protection have lower TB burdens. Progress on both indicators will help to eliminate catastrophic costs for people with TB and their households.
- Goal 2: End all forms of malnutrition. Undernutrition weakens the body’s defence against infections. Undernutrition is the biggest risk factor for TB, accountable for 2.3 million cases of TB in 2018.
- Goal 4: Quality education. Out-of-pocket costs associated with TB can force families to choose between buying food and paying for transport to the health centre, or paying their child’s school fees.
- Goal 7: Affordable and clean energy. Indoor air pollution, for example from cooking fuels, is a risk factor for TB.
- Goal 8: Economic growth and decent work for all. Preventing lost work hours due to TB globally will add US $12 billion to achieving sustainable economic growth and full productive employment. Historic trends in TB incidence are closely correlated with changes in the absolute level of GDP per capita. Moreover, certain jobs can put people at greater risk of developing TB, such as mining.
- Goals 5 and 10: Gender equality and reduced inequalities. TB is most prevalent among the poorest and most marginalised people in society. As shown in figure 2, gender has an impact on susceptibility to disease and well as likelihood of access treatment and being successfully treated.
- Goal 11: Sustainable cities and communities. TB incidence is linked to living conditions, for example people are at greater risk of developing TB if they live in an overcrowded or poorly ventilated environment.
This UHC Day, it is important to highlight interventions that support the “practical implementation” of UHC. For example, national governments and donors can practically implement the TB response to make it “universal.” Practically, there are two key opportunities for this, through influencing a country’s National Strategic Plan for TB and through influencing what is included in its funding request to the Global Fund. With the theme of Keeping the Promise today, here are a few ways national governments and donors can start delivering:
- Ministries and agencies across government, including health, social protection, labour, finance and education, must collaborate to ensure that the TB response holistically addresses the disease and its causes.
- Social protection interventions must be incorporated into national TB and UHC strategies. Interventions must target the causes of out of pocket costs and the issues preventing people accessing the care they need.
- In making applications to the Global Fund for renewed funding for the 2020-2022 period, social support services must be funded to make sure that all people can access TB diagnosis, treatment and care without experiencing out of pocket costs.
For more information, please see the latest RESULTS UK report “Tuberculosis & Universal* Health Coverage. *Terms and Conditions Apply.”